Psoriatic arthritis is a chronic inflammatory joint disease strongly linked to psoriasis and driven by immune system dysregulation. In many patients, joint symptoms develop gradually over time rather than appearing suddenly, which means early warning signs are sometimes overlooked. As a result, diagnosis may be delayed, even though early treatment plays a major role in preventing long-term joint damage and preserving mobility.
If you are new to the condition or want a full medical overview, you can start with our complete guide to psoriasis causes, symptoms, and treatment options.
Understanding how psoriatic arthritis develops helps patients recognize early symptoms and seek treatment before permanent joint damage occurs.
What Is Psoriatic Arthritis and Psoriasis Connection?
Psoriasis is now widely recognized as a systemic inflammatory condition rather than a disease affecting only the skin. Because of this systemic immune activation, inflammation can also affect joints, tendons, and connective tissue throughout the body. In addition, inflammatory signaling molecules such as cytokines help drive chronic inflammation, which explains why skin and joint symptoms often develop together in psoriatic disease.
Key biological drivers include:
Overactivation of T-cells
Inflammatory cytokines (TNF-alpha, IL-17, IL-23)
Chronic systemic inflammation
This systemic inflammation explains why psoriasis is now recognized as a whole-body inflammatory disease, not only a skin condition.
You can better understand how inflammation cycles start and worsen symptoms in this article about psoriasis triggers and flare causes.
Early Joint Warning Signs in Inflammatory Psoriatic Disease
Early symptoms of psoriatic arthritis often develop slowly and may initially seem mild or nonspecific. For example, patients may notice morning stiffness, mild joint swelling, or discomfort in the fingers, toes, or heels. Over time, however, persistent inflammation can begin to damage joint structures, which is why early recognition and evaluation are critical for long-term joint protection.
Early Indicators Doctors Look For
Common early symptoms include:
Morning stiffness lasting longer than 30 minutes
Swollen fingers or toes (dactylitis)
Heel pain or Achilles tendon pain
Lower back stiffness
Persistent fatigue linked to inflammation
Nail changes may appear before joint symptoms. These include:
Nail pitting
Nail thickening
Nail lifting from the nail bed
If you are unsure whether symptoms are skin-only or systemic, review early signs in this guide to psoriasis symptoms and progression.
How Chronic Inflammation Damages Joints Over Time
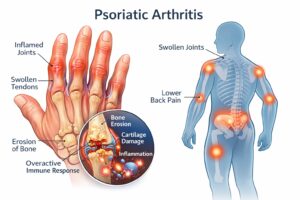
Psoriatic arthritis causes immune-driven inflammation that can damage joints, tendons, and surrounding connective tissue over time.
Chronic inflammation can gradually damage joint structures if it remains untreated. As inflammation progresses, cartilage and bone tissue may begin to deteriorate, leading to stiffness, reduced mobility, and structural joint damage. Therefore, modern treatment strategies focus on controlling immune activity early in the disease process to help prevent irreversible joint changes.
Immune Pathways Behind Joint Damage
Long-term uncontrolled inflammation can lead to:
Cartilage breakdown
Bone erosion
Joint stiffness and mobility loss
Permanent joint deformity in advanced disease
Modern treatments target immune pathways to stop structural joint damage, not only reduce pain.
According to research by PubMed, early diagnosis and treatment dramatically improve long-term outcomes and quality of life.
Lifestyle and Metabolic Factors That Increase Joint Risk
Lifestyle and metabolic factors can significantly influence inflammatory activity in psoriatic disease. In addition to genetic and immune factors, obesity, smoking, chronic stress, and poor sleep quality may increase the risk of symptom flares and disease progression. For this reason, many treatment plans include lifestyle management alongside medical therapy to help reduce overall inflammatory burden.
Inflammation Amplifiers in Daily Life
Obesity and metabolic syndrome
Chronic psychological stress
Smoking
Poor sleep quality
Diet high in ultra-processed foods
Nutrition and metabolic balance can support medical treatment. Learn more in this guide about psoriasis and diet interactions.
You can also explore common inflammatory foods in this article on foods to avoid with psoriasis.
When Joint Pain May Signal Systemic Disease
Joint pain should never be ignored in people living with psoriasis, especially if symptoms persist or worsen over time. However, not all joint discomfort is related to inflammatory arthritis, which is why proper medical evaluation is essential. Therefore, patients who experience ongoing stiffness, swelling, or tendon pain should seek medical assessment to rule out psoriatic arthritis or other inflammatory joint conditions. Look for signs of:
Persistent joint pain
Morning stiffness
Swollen fingers or toes
Tendon or heel pain
Reduced joint mobility
Which Specialists Evaluate Inflammatory Joint Disease
Diagnosis may involve:
Primary care physician initial evaluation
Rheumatology confirmation and treatment planning
Dermatology coordination for skin disease management
Testing may include inflammatory blood markers, ultrasound, or MRI imaging.
Systemic Conditions Linked to Psoriatic Disease
Psoriatic disease is associated with an increased risk of several systemic health conditions. Because chronic inflammation affects multiple body systems, patients may have a higher likelihood of developing cardiovascular disease, metabolic syndrome, and certain mental health conditions. In addition, inflammatory pathways linked to psoriatic disease may contribute to other autoimmune or inflammatory disorders.
Cardiovascular disease
Metabolic syndrome
Depression and anxiety
Inflammatory bowel disease
You can learn more in this overview of psoriasis associated conditions.
Long-Term Outlook With Modern Immune Therapies
With early diagnosis and modern immune-targeted therapies, many patients maintain active and independent lives. Monitoring symptoms, managing inflammation, and maintaining consistent medical follow-up are essential parts of long-term disease control.
Modern immune-targeted therapies have significantly improved long-term outcomes for many people living with psoriatic arthritis. In many cases, early diagnosis and consistent treatment help preserve joint function and reduce disease progression. As a result, many patients are able to maintain active lifestyles and good quality of life with appropriate medical care and long-term disease monitoring.
FAQs
1. Can you have psoriatic arthritis without psoriasis?
Yes. Some patients develop joint symptoms before visible skin symptoms appear.
2. Is psoriatic arthritis permanent?
It is a chronic condition, but early treatment can slow progression and prevent severe joint damage.
3. What age does psoriatic arthritis usually start?
Most commonly between ages 30 and 50, but it can develop at any age.
4. Is psoriatic arthritis the same as rheumatoid arthritis?
No. Both are autoimmune arthritis types, but they involve different immune pathways and joint patterns.
5. Does stress make psoriatic arthritis worse?
Yes. Chronic stress can increase inflammatory activity and trigger symptom flares.